Can you have dental implants with gum disease?

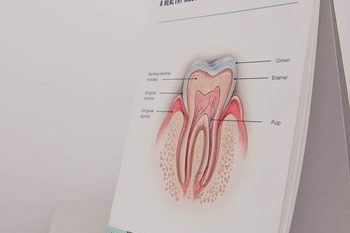
Gum disease can progress in stages; from subtle inflammation and bleeding (gingivitis), to more severe symptoms like gaps, receding gums, and loose teeth (periodontitis). The advanced stage of periodontitis will lead to loss of teeth and bone surrounding, bad breath and abscesses. In order to be a viable patient for dental implants your mouth needs to be in a healthy condition. Therefore, if you have active gum disease, you will not be able to have dental implants.
Can gum disease affect dental implants?
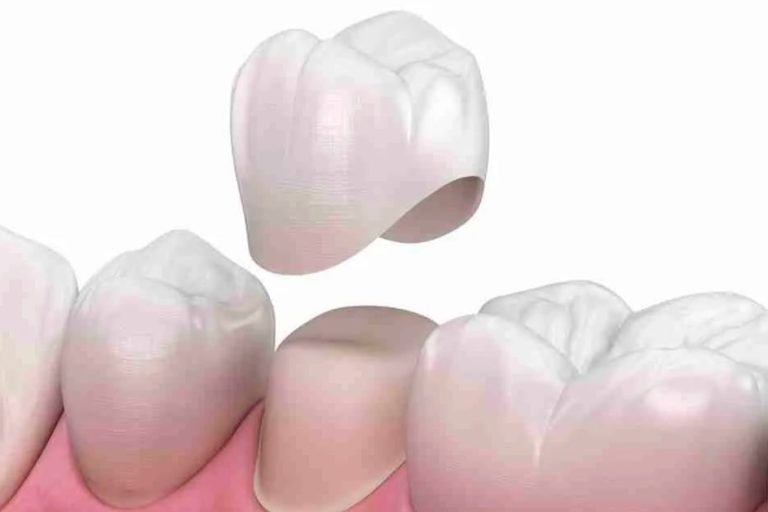
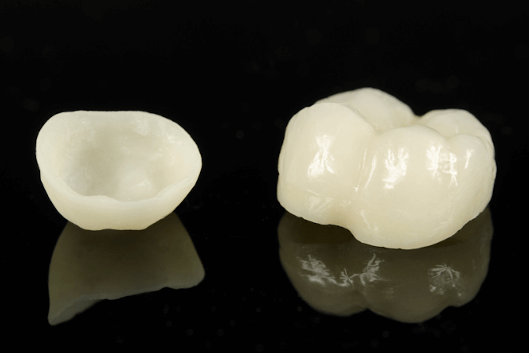
Yes, developing gum disease after you have had dental implants can affect them. The term used by dentists to describe the specific form of gum disease that can affect dental implants is peri-implantitis. There is also another condition called peri-implant mucositis, which is a condition similar to gingivitis, described as a reversible inflammatory lesion affecting the soft tissue in the area immediately around implants. The peri-implantitis instead will affect the soft tissue surrounding an implant and will be accompanied by bone loss.
When well looked after, dental implants can last a lifetime but, if they are not, they can become infected just like natural teeth and they can get affected to the point of loss. You may be wondering how this can happen if they are not natural and unable to get decayed? Well, the answer is that dental implants can become diseased or fail if they are neglected or do not receive regular care from a dental professional.
Like periodontitis, this infection can be the result of smoking, poor oral hygiene, diabetes, bite problems, parafunctional habits (bruxism), or non-integration of the implant itself. If left untreated, the progressive bone loss and infection can cause the implant to fail.
How do you know if your dental implant is failing?
The symptoms can be similar to those of gum disease and can include one or more of the following symptoms:
- loose or wobbly implant,
- red or puffy gums around the implant,
- icky taste,
- bad breath,
- throbbing pain or discomfort from the area,
- dull ache on palpation,
- exudate (pus) visible from the area,
- threads are visible on the implant,
- difficulty chewing,
- fever, or
- bleeding when brushing around the implant.
With your regular visits your dentist can diagnose peri-implantitis quickly with a clinical exam and a radiograph. The long-term goal is to arrest the progression of the infection and maintain the implant.
How is Peri-implantitis treated?
Depending on the level of infection, your dentist may prescribe special mouth rinses or present a combination of other options to get your implant back on a healthy track. There are many treatment options that may include antibiotics, surgery, laser therapy with surface decontamination, mechanical debridement, or antimicrobial therapy.
You must not ignore peri-implantitis, it can be destructive and aggressive. An infected implant can lead to more serious illness, that can cause damage to the heart and other body organs. If left untreated long enough, low-grade bacterial infections can have serious consequences.
As dentists, we want you to be healthy. If you suspect an infected implant, contact your dentist immediately so the appropriate treatment can be started sooner rather than later. Once your implant is healthy again, keep up with your new hygiene regime.
Call 020 3925 3846 or fill in our form to enquire about your consultation.